People, Processes, & Disciplines of Clinical Data Management
Last week I had the pleasure of attending the ACDM conference in Copenhagen, Denmark. On my return to the UK I started to wonder if the term Clinical Data Management (CDM) is clearly understood. In my opinion it does not only refer to the people and processes of running a clinical trial, but it should also encompass the software required to manage clinical trials. This post asks what does CDM mean and is designed to describe the components of a trial that are handled but is by no means a comprehensive description of all aspects of running clinical trials.
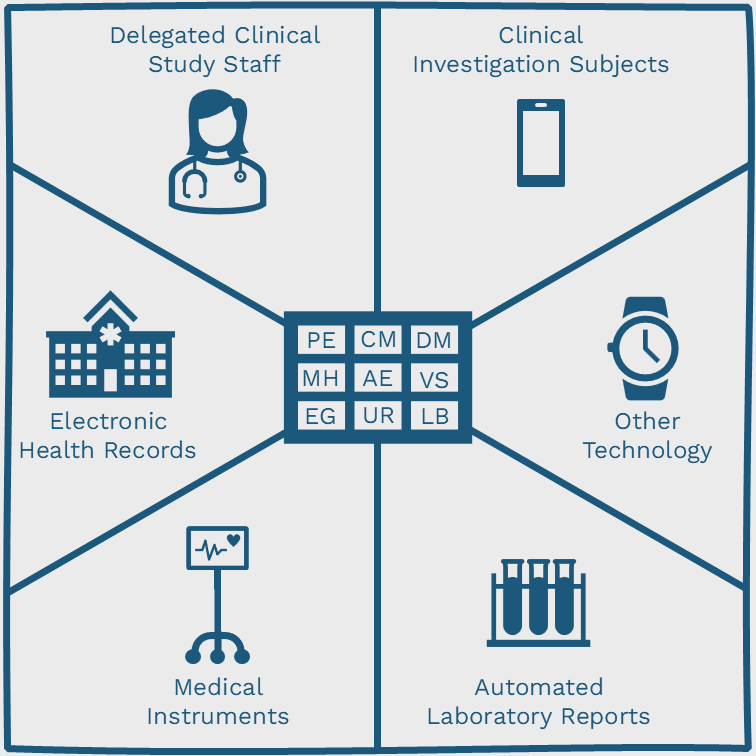
Therefore my definition of Clinical Data Management (CDM) is a broad term used to describe the group of people, processes, and disciplines that are actively involved in all stages of clinical trials.
The software tools used by CDM teams are collectively referred to as Clinical Data Management Systems (CDMS); and include components such as CTMS, eTMF, eSource, EDC, eConsent, eCOA, RTSM, Coding, RBQM, and Analytics. Some products include multiple components but very few will include everything used by a CDM team to manage the whole trial.
The following components of a trial (often referred to as a study) are typically handled by CDM but responsibilities can overlap across teams, depending on the organisation size.
- Case Report Form (CRF) design and annotation
- Data-entry and data validation
- Discrepancy management
- Medical coding
- Data extraction and database locking
CRF design historically refers to the creation of a paper form for data to be entered onto at the point of care. However, more recently this term is used interchangeably to describe the ability to build forms within an Electronic Data Capture (EDC) system.
CRF annotations are variables from the Study Data Tabulation Model (SDTM) implementation guide that are laid over the top of the CRF. The over-lay of variables allows data managers to ensure data entry fields are mapped to a standard output format which will facilitate the statistical review of collected data.
Data-entry is performed from paper into the CRF, and data validation is the process of confirming data is entered according to specifications outlined in the study protocol.
A study protocol is a document created by the sponsor that describes the objectives, design, methodology, and statistical considerations required to organise a clinical trial. The protocol ensures the safety of subjects participating in the trial and ensures data is collected with integrity. Additional documents that accompany the protocol include instructions for lab sample processing, a manual of operations, a plan for statistical analysis, the approach for monitoring safety; and various reports required to demonstrate study activities and outcomes.
A discrepancy is a deviation from the protocol and must be managed to ensure data is cleaned before submission. This process is also referred to as query resolution and should be included in any system used to electronically capture data, along with a comprehensive audit trail of changes.
Medical coding is performed on data that has been collected and helps categorize information so that it can be analysed and reviewed. Typically, coding is performed by searching medical dictionaries such as MedDRA and WHO Drug then selecting the term most relevant to the verbatim description.
Data extraction refers to the process of exporting data from the study to industry standard formats such as SAS (Statistical Analysis System) transport files; or to a self-contained ODM (Operational Data Model) file.
Database locking occurs at the end of a trial and involves making sure all queries are resolved before consulting with the statistician and finalising SAS datasets. After a period has passed, the database must be archived.